Optimize Physician Productivity To Improve Your Bottom Line
Table of Contents
Managing a successful medical practice in today’s healthcare climate requires navigating a host of challenges: complicated government regulations, partner service agreement expectations, Covid-related volume and revenue losses, and growing consolidation efforts. Now, more than ever, practice leadership must thoroughly evaluate revenue-generating opportunities to maintain financial health and independence. Common initiatives include regional expansion, added service lines, improved quality of care, and productivity optimization.
There is a growing focus on provider productivity as organizations explore ways to leverage existing resources to meet growing volume demands, control operational expenses, and improve affordability of services
Let’s take a look at a few aspects of productivity that, when monitored and handled properly, can directly impact your bottom line:
Compensation
Many compensation models measure physician productivity in relative value units (RVUs). A more valid approach involves a holistic view of productivity. In a recent blog post, Quinsite CEO Jeff Maze discusses how practices can move from tracking traditional RVU productivity towards measuring total provider value, which incorporates both time spent as well as level of difficulty and effort. He also emphasizes the importance of capturing valuable non-RVU productivity that often goes unrecognized yet impacts quality of care and overall practice success (i.e., E&M consults, patient/family education, board meetings, networking, and administrative time)
Staffing
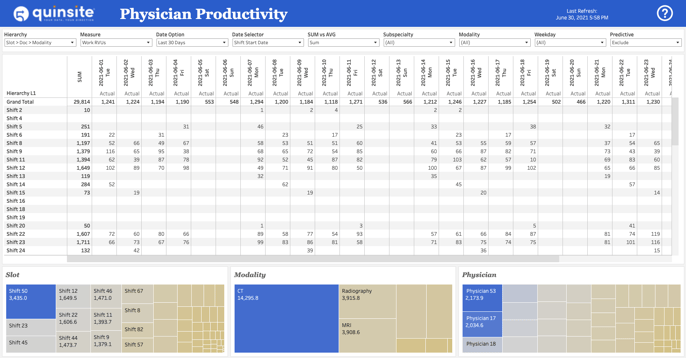
Properly labeling, capturing, and measuring physician productivity can help your practice understand total labor costs, as well as compare overall staffing levels against patient/service demand to identify potential staffing gaps or opportunities to increase productivity within your existing pool of resources.
Supply vs Demand
As mentioned above, using healthcare data analytics services to compare patient volumes to productivity levels by days/times/locations can help your practice better understand demand for services and make impactful adjustments such as changing/adding services, hours of operation, shift structures, and more.
Partner & Provider Expectations
Physician productivity varies widely across each organization depending on shift, location, department, specialty, support staff, etc. When it comes to partner agreements, a solid understanding of these details helps you set realistic service goals to ensure that partner expectations are clear, reasonable, and attainable. Furthermore, the ability to track and compare individual productivity against practice benchmarks offers valuable performance feedback to help guide discussions around provider expectations and accountability and support better data driven decision making in healthcare.
Growth/Sustainability
Examining historical productivity data and tracking current productivity data (another example of predictive analytics in healthcare) can help you establish benchmarks, forecast growth, and make data-driven decisions about your practice’s strategic direction.
Real Results
Mountain Medical Physician Specialists offers a great example of how enhanced visibility into physician productivity empowered physicians to improve their individual performance. Using the Productivity Ring tool in Quinsite’s mobile app, the practice realized a 15% increase in average daily RVU's per physician while also achieving a more equitable spread of daily workloads across all providers. In addition to generating more revenue, expansion of existing practice capacity eliminated the urgent need for hiring another FTE (approximately $500,000), even in the face of increased volumes. Read the case study here.
In summary, there are several important steps we recommend to help your practice improve overall understanding of productivity for the purpose of increasing outputs to improve quality of service, reduce costs, and generate more revenue in addition to supporting better data driven decision making in healthcare:
- Integrate data from disparate systems: Many of your systems are rich with valuable data, yet they don’t talk to each other. If your primary reporting process isn’t capturing 100% of work performed or time/effort spent then your practice is not only at risk for leaving money on the table, it will impair your ability to accurately compare individual provider performance to practice benchmarks.
- Capture and track non-RVU time: Utilize a holistic view of productivity. Read our blog post on compensation to learn more.
- Pay attention to the details: Capture all aspects of revenue-generating work (shift, location, department, specialty, etc) to understand their individual impact to productivity for improved strategies (i.e., day shift tends to get more interruptions and are less productive vs evening or night shift, inpatient locations get more interruptions and are less productive vs outpatient).
- Leverage robust productivity reporting: Whether you utilize in-house analysts or outsourced tools/resources, proper visibility into practice productivity pays for itself in new revenue generation and cost savings.
- Share the data: Enhance partnerships and empower physicians by providing ongoing feedback about performance, including practice benchmarks, clear expectations, and comparison to peer performance.
Discover how to unleash the power of your data.



